Deep Dive: What is Extracorporeal Membrane Oxygenation (ECMO)?
Deep Dive: What is Extracorporeal Membrane Oxygenation (ECMO)?
During the pandemic, as doctors and researchers scrambled for ways to save lives and fight back a brand new virus wreaking havoc on patients, a four-letter acronym gained new attention in the mainstream press.
ECMO (Extracorporeal membrane oxygenation) became an increasingly relied-upon therapy for some of the sickest COVID-19 patients, a potential lifeline to recovery when options were limited. But the therapy has existed for decades before the arrival of COVID-19 and remains an invaluable second chance for patients who are critically ill with a variety of diseases and conditions.
But what exactly is ECMO? Let’s break it down:
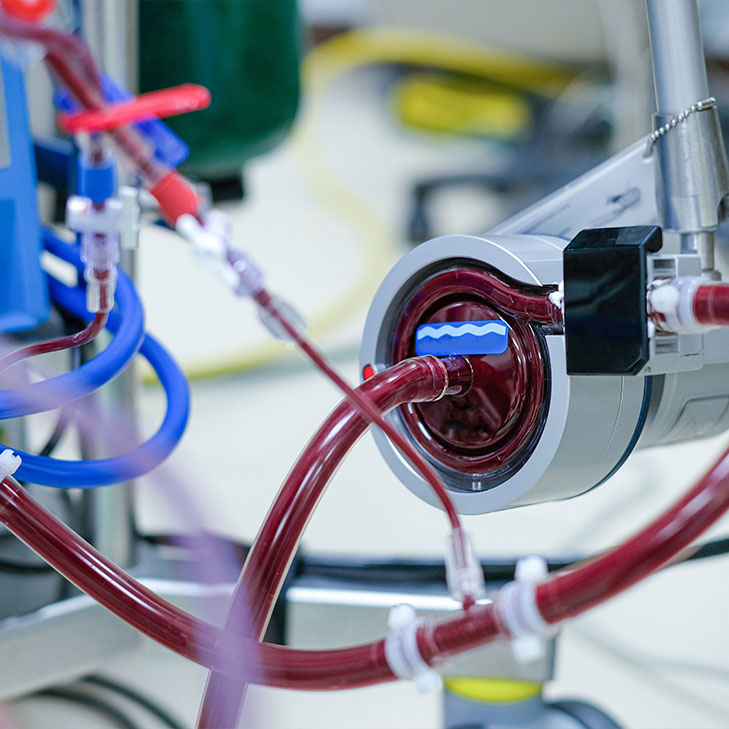
Essentially, ECMO does the job of your heart and lungs so they don’t have to. During ECMO, blood is actually pumped outside of the body to a specialized machine that not only oxygenates it, but removes carbon dioxide before it is then pumped back into the body. That means that for patients with severe cardiac or respiratory failure—or patients in shock or a coma—the heart and lungs can rest and heal while their critical functions remain uninterrupted.
While it doesn’t treat or cure disease on its own, it can buy valuable time and the ability to provide oxygen when the body is unable to provide it for itself.
Patients on ECMO receive pain medication and sedatives, and while they may be unconscious for the procedure, some patients may also be awake and be able to interact with their doctors and loved ones. The duration may be as short as a few hours, or it could be as long as weeks, depending on the patient and the condition and treatments ECMO is being used to address—but doctors always try to get patients off ECMO as soon as possible.
An ECMO machine has several parts: a pump keeps the blood moving, an artificial lung adds oxygen and removes carbon dioxide, a blood warmer maintains temperature, and a filter ensures the blood is clean. There are also two types of ECMO machines. Veno-arterial (VA) ECMO, simulates both heart and lung function, while Veno-venous (VV) ECMO just supports lung function without cardiac support.
At Texas IPS, we are fully equipped to provide life-saving support for critically ill patients, and we have some of the region’s leading experts in ECMO among our physicians. We are also proud to work with the Institute for Extracorporeal Support to lead the conversation and education on ECMO from an industry perspective, sharing our knowledge and improving patient outcomes in our facilities and beyond.
To learn more about ECMO, click here.
About Texas IPS
Texas IPS, based in San Antonio, is an independent physician owned medical practice specializing in the treatment of pulmonary, sleep, and critical care medicine. Texas IPS’ knowledgeable physician staff is composed of highly trained clinicians dedicated to providing high quality care through a patient centered approach using advanced technology and innovation.