Busting the biggest COPD myths
Busting the biggest COPD myths
Although 16 million Americans have been diagnosed with chronic obstructive pulmonary disease, it remains remarkably misunderstood, even to some people already suffering.
Let’s tackle those misconceptions head on. But first, a primer on COPD:
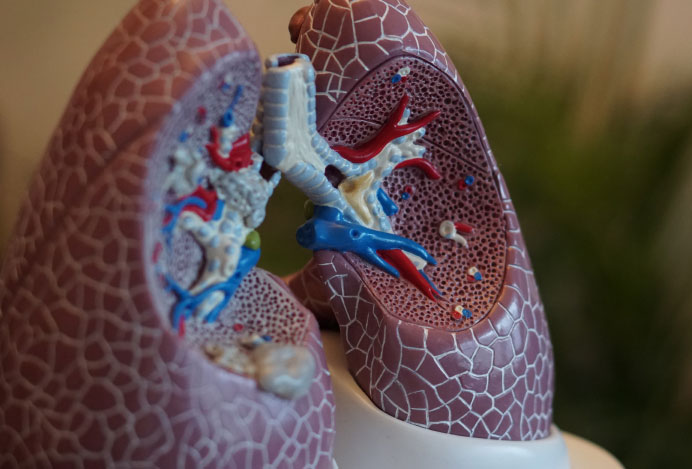
COPD has two main forms, with many patients experiencing both at the same time. The first is chronic bronchitis, an inflammation of the breathing tubes that can constrict airways. The second is emphysema, or damage to the alveoli (delicate air sacs) in the lungs. When alveoli are damaged, they carry less oxygen to your blood and trap stale air in your lungs.
Symptoms often include a cough and shortness of breath, starting off mild and getting worse over time, especially if left untreated.
Now, let’s turn to the myths:
- Only smokers get COPD: Smoking may be the leading cause of COPD, but it isn’t exclusively a smoker’s disease. About 10-20% of COPD patients, in fact, never smoked. Other risk factors include exposure to second-hand smoke and air pollution, some forms of asthma, and alpha-1 antitrypsin deficiency, which is an enzyme that helps protect against immune attacks. Those with alpha-1 antitrypsin deficiency can be at higher risk of developing COPD.
- Young people can’t develop COPD: While it’s true that younger people may be less likely than older adults to develop COPD, the disease isn’t unheard of in younger generations. According to the CDC, COPD affects 2% of men and 4.1% of women ages 24-44 and 2% of men and 3% of women from 18-24.
- COPD is strictly a pulmonary disease: COPD often occurs—and could even be partially caused by—several comorbidities, including high blood pressure, heart disease, lung cancer, and diabetes. At the same time, COPD causes your heart to work harder and beat faster, putting patients at a greater risk for subsequent heart attack and heart disease.
- There’s no point in quitting smoking if you have COPD: It is never too late to quit smoking, period. Smoking quickens the progression of COPD, and while the lung damage from COPD isn’t reversible, further damage can be prevented through quitting, especially in early stages.
- You can’t exercise if you have COPD: Physical exercise may be difficult without the proper support, but pulmonary rehabilitation can help increase lung capacity to improve quality of life and enable more physical activity.
- COPD can’t be treated: There isn’t a cure for COPD, but treatments—especially in early stages—can dramatically improve quality of life and slow disease progression. Supplemental oxygen can help treat emphysema, and chronic bronchitis can be treated with bronchodilators and corticosteroid inhalers.
A COPD diagnosis can be scary, but it can be managed—with the right help. At Texas IPS, we provide state-of-the-art care and personalized treatment plans for every patient. We want you to breathe easier and feel strong.
Interested in learning more? Reach out to schedule an appointment today.
About Texas IPS
Texas IPS, based in San Antonio, is an independent physician owned medical practice specializing in the treatment of pulmonary, sleep, and critical care medicine. Texas IPS’ knowledgeable physician staff is composed of highly trained clinicians dedicated to providing high quality care through a patient centered approach using advanced technology and innovation.